KNEE CARTILAGE REPAIR PERTH
Knee Cartilage Repair Surgery – A patient’s guide:
Australian Academy of Robotic
Orthopaedic Surgeons

What is Knee Cartilage
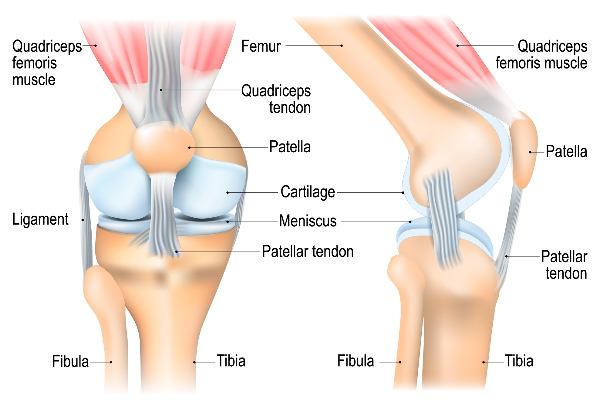
Your knee joints are lined by extremely smooth tissue called cartilage.
The cartilage of the knee joint lines:
The cartilage is a protective cushion, allowing smooth movement of the joints as one bone end moves on the other.
Cartilage tissue covers the adjacent bone surfaces of the knee.
Knee Cartilage Repair Surgery – Aim
The aim of knee cartilage repair surgery is to:
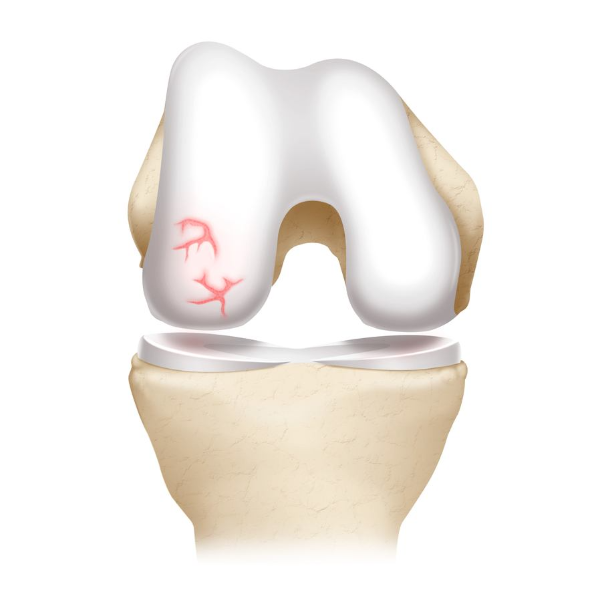
The size and location of the cartilage damage (or lesion) in the knee joint and the status of the other structures within the knee joint will help determine whether surgery is possible/suitable for your unique diagnosis.
Other structures within the knee may need to be assessed including, knee alignment, ligaments, cartilage damage or other factors.
These assessments will help identify patients who are more or less likely to benefit from the surgery and help determine the best surgical approach.
Further knee joint assessment
Further investigations of the knee joint may reveal other structures in need of removal, trimming or repair including:
Further knee assessment tests may include x-rays, ultra-sound or MRI or CT scan.

Types of Knee Cartilage Repair Surgery
There are five main types of knee cartilage repair surgery.
The benefits and risks of the most appropriate surgical approach to your unique situation will be discussed with you, by your surgeon to ensure you have all the information to make an informed decision about your diagnosis and treatment options.
Please access the buttons below to find out more about the main knee cartilage repair surgical approaches:
After Knee Cartilage Repair Surgery
Recovery times may vary from patient to patient for a number of reasons including age, current heath, surgical complexity, muscle and bone strength and commitment to rehabilitation amongst many other factors.
Surgery – The surgery itself usually takes 1 – 2 hours.
Post-surgery – For some patients it’s day surgery, so you will be observed for a couple of hours to ensure that you have recovered from the anaesthetic and discharged from hospital.
Some patients will stay overnight in hospital.
After surgery you will probably feel a bit sleepy and might need some pain killers. Have a friend or family member available to help you for a few days after you leave hospital.
You will be given instructions on:
What are the Risks of Knee Cartilage Repair Surgery
Potential risks knee of knee cartilage repair surgery – Knee cartilage repair surgery is very safe, and serious complications are uncommon. The surgeries have a high success rate in reducing pain and improving knee function and mobility.
It may take several months to a year for the full benefits of the procedure to be realised. Some patients may need additional surgeries or treatments to manage symptoms in more complex cases.
As with any major surgery, there are potential risks involved. The decision to proceed with the surgery is made because the advantages of surgery outweigh the potential disadvantages.
It is important that you are informed of these risks before the surgery takes place. Complications can be medical (general) or local complications specific to the knee. Medical complications include those of the anaesthetic and your general well being. Almost any medical condition can occur so this list is not complete.
Complications that may include:

